Allergy Skin Test
Skin Testing Methods and Standards (ACAAI)
Board-certified allergists are specialists who are highly trained to understand the ins and outs of allergy
testing and to oversee what happens during and after test sample analysis. These skills are important
because there are many variables that affect allergy test results. If these nuances are missed or wrongly
interpreted by physicians who do not specialize in allergies and asthma, individuals may not get the best
treatment to relieve their symptoms.
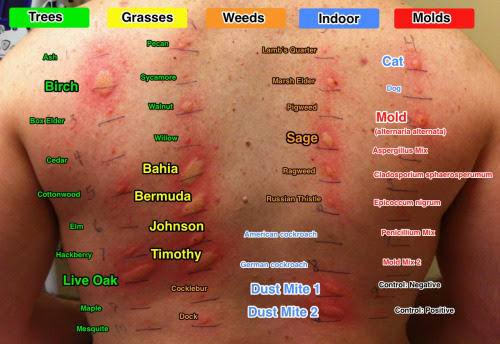
Skin tests for allergic disorders have been around since the 1860s. Today, prick or puncture tests are
commonly used by allergists as diagnostic aids. These tests are not very invasive and, for most allergens,
they tend to produce quick results. If the results of prick or puncture tests are negative, they may be
followed by intradermal tests, which give allergists more details about what’s causing the underlying
symptoms.
Here is how both types of tests are administered:
Prick/puncture – A diluted allergen is applied with a prick or a puncture on the surface of the skin.
Intradermal – Using a 26- to 30-guage (very thin) needle, a diluted allergen is injected immediately below
the skin surface.
After either type of test, the area of the skin is observed for about 15 minutes to see if a reaction
develops. The “wheal”—a raised, red, itchy bump and surrounding “flare”—indicates the presence of
the allergy antibody when the person is exposed to specific allergens. The larger the wheal and flare, the
greater the sensitivity.
Although skin testing may seem simple, it must be carried out by trained practitioners with an
understanding of the variables and risks of the testing procedure.
Steps should include:
After reviewing the patient’s medical history and performing a physical exam, the allergist determines
that allergy skin testing is both appropriate for the patient and does not put the patient at risk for a bad
outcome (such as severe anaphylaxis or an asthma attack in poorly controlled asthma).
A trained staff performs the skin testing under the supervision of the allergist.
The allergist personally “reads” the skin tests and, in evaluating the skin test reactions, discerns several
factors that lead to proper interpretation.
These factors include:
- Proper evaluation and selection of which patient may benefit from skin testing
- Condition and reactivity of the skin
- Proper selection of where the skin tests are placed
- Type of skin test placed
- Device used for skin testing
- Proper technique in applying the tests
- Quality and selection of the allergen extracts used
- Medications that could alter the validity of the results
Reporting Standards
In addition to carefully considering allergy testing variables, board-certified allergists are trained to
report test results according to standard practices endorsed by the American College of Allergy, Asthma
& Immunology.
Standardized allergy test records are vital since patients often change doctors. When they do, their new
allergist must be able to accurately interpret their health records. If information is incomplete, patients
may be ordered to undergo additional skin testing that would have been unnecessary had standard
practices been followed.
Guidelines suggest that skin test records report the diameter of the wheal and the surrounding “flare”
(measured in millimeters) and record information to account for the differences in testing devices. The
measurements are usually reported in millimeters of diameter.
Allergy staff performing allergy and asthma tests are also required to meet basic quality assurance
standards to ensure that they are using the proper techniques.
Seeing a board-certified allergist will assure these guidelines are followed. Allergy skin testing is
relatively safe; adverse reactions are rare. Even so, researchers recommend that the value of any test be
carefully considered before it is administered.